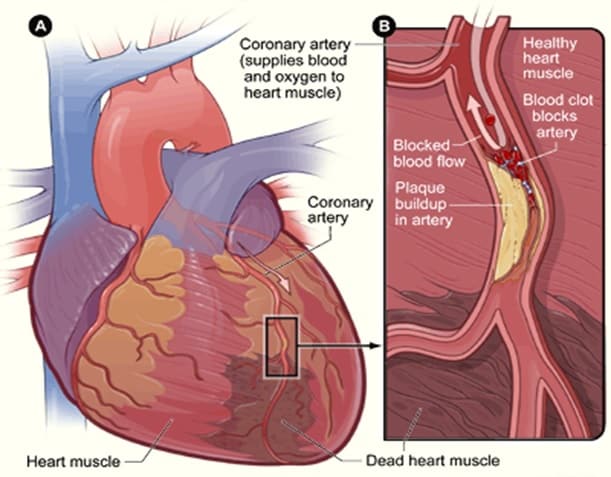
 Coronary artery disease is a condition in which fatty deposits (atheroma) accumulate in the cells lining the wall of the coronary arteries. These fatty deposits build up gradually and irregularly in the large branches of the two main coronary arteries which encircle the heart and are the main source of its blood supply. This process is called atherosclerosis which leads to narrowing or hardening of the blood vessels supplying blood to the heart muscle (the coronary arteries ). This results in ischemia ( inability to provide adequate oxygen) to heart muscle and this can cause damage to the heart muscle . Complete occlusion of the blood vessel leads to a heart attack (myocardial infarction). Exact cause is unknown. However there are a number of risk factors. Control of these risk factors has been shown to reduce the severity and complications of the disease.
Coronary artery disease is a condition in which fatty deposits (atheroma) accumulate in the cells lining the wall of the coronary arteries. These fatty deposits build up gradually and irregularly in the large branches of the two main coronary arteries which encircle the heart and are the main source of its blood supply. This process is called atherosclerosis which leads to narrowing or hardening of the blood vessels supplying blood to the heart muscle (the coronary arteries ). This results in ischemia ( inability to provide adequate oxygen) to heart muscle and this can cause damage to the heart muscle . Complete occlusion of the blood vessel leads to a heart attack (myocardial infarction). Exact cause is unknown. However there are a number of risk factors. Control of these risk factors has been shown to reduce the severity and complications of the disease.
Coronary artery disease is a chronic process that begins during adolescence and slowly progresses throughout life. Independent risk factors include a family history of premature coronary artery disease, cigarette smoking, diabetes mellitus, hypertension, hyperlipidemia, sedentary lifestyle, and obesity. These risk factors accelerate or modify a complex and chronic inflammatory process that ultimately manifests as fibrous atherosclerotic plaque.The most widely accepted theory of atherosclerosis states that the process represents an attempt at healing in response to endothelial injury. The first step in the atherosclerotic process is the development of fatty streaks, which contain atherogenic lipoproteins and macrophage foam cells.
These streaks form between the endothelium and internal elastic lamina. Over time, an intermediate lesion made up of an extracellular lipid core and layers of smooth muscle and connective tissue matrix eventually forms a fibrous cap. The edge of the fibrous cap (the shoulder region) plays a critical role in the development of acute coronary syndromes. The shoulder region is the site where most plaques lose their integrity, or rupture. Plaque rupture exposes the underlying thrombogenic core of lipid and necrotic material to circulating blood. This exposure results in platelet adherence, aggregation, and progressive luminal narrowing, which are associated with acute coronary syndromes.Inflammation is emerging as a critical component of atherosclerosis genesis, activity, and potential plaque instability.
Patients with established coronary artery disease who possess a confluence of risk factors known as the metabolic syndrome remain at particularly high risk for a future vascular event, such as an acute myocardial infarction or cerebrovascular accident. Biochemical markers such as elevated levels of C-reactive protein signal a higher likelihood of vascular inflammation and portend a higher risk of vascular event rates. This marker may also signal more rapidly advancing coronary artery disease and the need for aggressive preventive measures.
