Introduction
The schizophrenia spectrum and other psychotic disorders is the general categorization for the disorder that I have chosen which is schizophrenia. Some key features that define the schizophrenia spectrum and other psychotic disorders category are delusions, hallucinations, disorganized thinking (speech), grossly disorganized or abnormal motor behavior (including catatonia), and other negative symptoms (negative symptoms referring to symptoms that subtract, like diminished emotional expression).
While I am focusing on schizophrenia there are other disorders in this category such as: Schizotypal (Personality) Disorder, Delusional Disorder, Brief Psychotic Disorder, Schizophreniform Disorder, Schizoaffective Disorder, Substance/Medication-Induced Psychotic Disorder, Psychotic Disorder Due to Another Medical Condition, Catatonia, Catatonia Associated With Another Mental Disorder (Catatonia Specifier), Catatonic Disorder Due to Another Medical Condition, Unspecified Catatonia, Other Specified Schizophrenia Spectrum and Other Psychotic Disorder, and Unspecified Schizophrenia Spectrum and Other Psychotic Disorder.
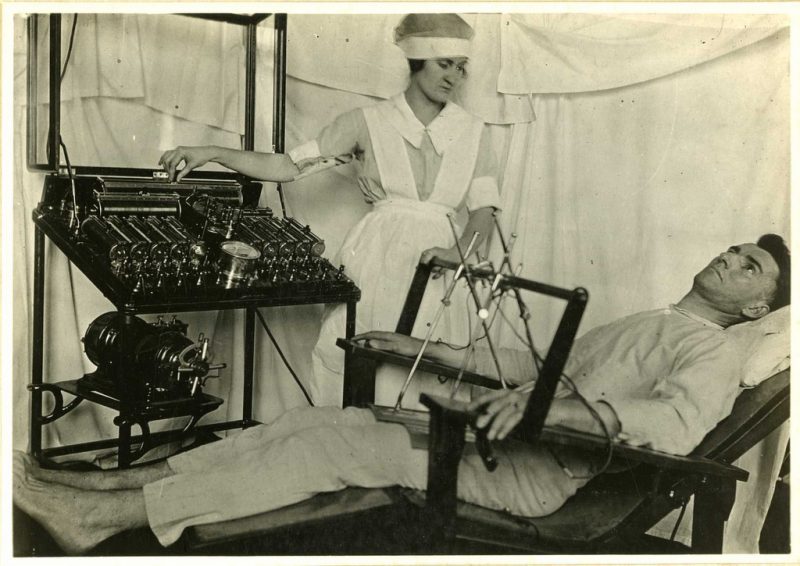
History of Schizophrenia
The term ‘schizophrenia’ was coined in 1910 by the Swiss psychiatrist Paul Eugen Bleuler, and is derived from the Greek words ‘schizo’ meaning split and ‘phren’ meaning mind. Bleuler had intended the term to refer to the dissociation or ‘loosening’ of thoughts and feelings that he had found to be a prominent feature of the illness.
Although schizophrenia sufferers may hear voices that they attribute to various people or have strange beliefs that seem out of keeping with their usual selves, this is not the same as having a ‘split personality’ despite the common belief that it is. The term ‘schizophrenia’ has led to much confusion about the nature of the illness, but Bleuler had intended it to replace the older, even more misleading term of ‘dementia praecox’ (or ‘dementia of early life’).
This older term had been championed by the German psychiatrist Emil Kraepelin, who mistakenly believed that the illness only occurred in young people and that it inevitably led to mental deterioration. Bleuler disagreed on both counts and, attempting to clarify matters, changed the name of the illness to ‘schizophrenia’. Bleuler believed that schizophrenia led to a heightened consciousness of memories and experiences, despite the ‘mental deterioration’.
Although Kraepelin had some mistaken beliefs about the nature of schizophrenia, he was the first person to distinguish the illness from other forms of psychosis, and in particular from the ‘affective psychoses’ that occur in mood disorders such as depression and manic-depressive illness (such as bipolar affective disorder). Kraepelin first isolated schizophrenia from other forms of psychosis in 1887, but this is not to say that schizophrenia, or ‘dementia praecox’, as he called it, had not existed long before Kraepelin’s day.
The oldest available description of an illness closely resembling schizophrenia can be found in the Ebers papyrus, which dates back to Egypt in 1550 BC. Not to mention archaeological discoveries of Stone Age skulls with burr holes drilled into them (presumably to release ‘evil spirits’) have led to speculation that schizophrenia is as old as mankind itself.
Diagnostic Criteria and Features of Schizophrenia
A. In order to be diagnosed with schizophrenia you need to have two or more of the following symptoms, each one has to be present for a significant portion of time during a one month period (it has been noted that the time period can be less if successfully treated). At the very least one of the “two or more” symptoms must be 1, 2, or 3.
- Delusions
- Hallucinations
- Disorganized speech (e.g., frequent derailment or incoherence)
- Grossly disorganized or catatonic behavior.
- Negative symptoms (i.e., diminished emotional expression or avolition)
B. For a significant portion of the time, since the onset, level of function in one or more major area, such as work, interpersonal relationships, or self care (such as hygiene, eating, sleeping, etc.), is noticeably below the level achieved prior to the onset (or when the onset is in childhood or adolescence, there is failure to achieve expected level of interpersonal, academic, or occupational functioning).
C. Continuous signs of the disease must persist for at least six months. This six month period must include at least one month of symptoms (or less if successfully treated) that meet the criteria of section A and may include periods of prodromal or residual symptoms. During these prodromal or residual periods, the signs of the disease may be manifested by only negative symptoms or by two or more symptoms listed in the criteria of section A present in an attenuated form (such as odd beliefs, unusual perceptual experiences).
D. Schizoaffective disorder and depressive or bipolar disorder with psychotic features must have been ruled out because 1 ) no major depressive or manic episodes have occurred concurrently with the active-phase symptoms, or 2) if mood episodes have occurred during active-phase symptoms, they have been present for a minority of the total duration of the active and residual periods of the illness.
E. The “disease” is not attributable to the physiological effects of a substance (such as drug abuse, or a medication) or another medical condition.
F. If there is a history of autism spectrum disorder or a communication disorder of childhood onset, the additional diagnosis of schizophrenia is made only if prominent delusions or hallucinations (in addition to the other required symptoms of schizophrenia) are also present for at least 1 month (or less if successfully treated).
Treatment of Schizophrenia
Schizophrenia requires lifelong treatment, even when symptoms have subsided. Treatment with medications and psychosocial therapy can help manage the condition. In some cases, hospitalization may be needed. A psychiatrist experienced in treating schizophrenia usually guides treatment. The treatment team also may include a psychologist, social worker (depending on the age of the patient and whether they have children or not), psychiatric nurse and possibly a case manager to coordinate care. The full-team approach may be available in clinics with expertise in schizophrenia treatment.

Medications are the cornerstone of treating a patient with schizophrenia. Antipsychotic medications are the most commonly prescribed drugs, they’re thought to control symptoms by affecting the brain neurotransmitter that controls your dopamine levels. The goal of treatment with antipsychotic medications is to effectively manage signs and symptoms at the lowest possible dose.
A psychiatrist may try different drugs, different doses, or combinations over time to achieve the desired result. Other medications also may help, such as antidepressants or anti-anxiety drugs. It can take several weeks to notice an improvement in symptoms. Because medications for schizophrenia can cause serious side effects, people with schizophrenia may be reluctant to take them.
Willingness to cooperate with treatment may affect drug choice. For example, someone who is resistant to taking medication consistently may need to be given injections instead of taking a pill.
Once psychosis recedes, in addition to continuing on medication, psychological and social (psychosocial) interventions are important. These may include: individual therapy, psychotherapy may help to normalize thought patterns. Also, learning to cope with stress and identify early warning signs of relapse can help people with schizophrenia manage their illness. Social skills training focuses on improving communication and social interactions and improving the ability to participate in daily activities.
Family therapy provides support and education to families dealing with schizophrenia. Vocational rehabilitation and supported employment focus on helping people with schizophrenia prepare for, find and keep jobs. Most individuals with schizophrenia require some form of daily living support. Many communities have programs to help people with schizophrenia with jobs, housing, self-help groups, and crisis situations. A case manager or someone on the treatment team can help find resources. With appropriate treatment, most people with schizophrenia can manage their illness.
