A disease characterized by variable, recurrent, reversible airway obstruction with intermittent episode of wheezing and dyspnea. It is associated with bronchial hypersensitivity and inflammation caused by various stimuli. Asthma is the most common chronic disease of childhood with 5% to 10% of school-aged children having symptoms of asthma. Asthma may develop on infants, but it usually develops after the third birthday. It is more common in urban settings.
Causes
- Pollen
- Animal dander
- House dust or mold
- Kapok or feather pillows
- Food additives containing sulfites and other sensitizing substance.
- Drugs and chemicals (e.g. aspirin, various non-steroidal anti-inflammatory drugs.)
- Exercise
- (Irritants, emotional stress, fatigue, exposure to noxious fumes, and endocrine, temperature, and humidity change may aggravate asthma attacks.)
Types of asthma
- Extrinsic asthma
Asthma that results from sensitivity to specific external allergens is known as extrinsic. Caused by inhaled allergens (e.g. dust, dust mites, mold, pollens, feathers, and animal dander.)
Extrinsic (atopic) asthma usually begins in childhood and is accompanied by other manifestations of atopy such as eczema and allergic rhinitis.
- Intrinsic asthma
Asthma that is caused by infection (often viral) and environmental stimuli (such as air pollution.)
- Mixed asthma
In which type 1 (immediate) reactivity appears to be combined with intrinsic factors.
- Aspirin-induced asthma
Caused by ingestion of aspirin related compounds.
- Exercise-induced asthma
In which respiratory symptoms occur within 5 to 10 minutes after exercise.
- Occupational asthma
Caused by industrial fumes, dust, and gases.
- Status asthmaticus
A severe form of acute asthma in which airway obstruction resists conventional drug therapy and lasts longer than 24 hours. Unless treated promptly. Other complications include pneumonia, atelectasis, dehydration, dysrrhytmias, cor pulmonale, respiratory failure and death.
ANATOMY AND PHYSIOLOGY
Nasal passages:
Air entering from the nostrils is led to the nasal passages. The nasal cavity that is located behind the nose comprises the nasal passages that form an important part of the respiratory system in human beings. The nasal cavity is responsible for conditioning the air that is received by the nose. The process of conditioning involves warming or cooling the air received by the nose, removing dust particles from it and also moistening it, before it enters the pharynx
Pharynx:
Located behind the nasal cavity and above the larynx. It is also a part of the digestive system of the human body. Food as well as air passes through the pharynx.
Larynx:
Associated with the production of sound. It consists of two pairs of membranes. Air causes the vocal cords to vibrate, thus producing sound. The larynx is situated in the neck of mammals and plays a vital role in the protection of the trachea.
Trachea:
The term refers to the airway through which respiratory air travels. The rings of cartilage within its walls keep the trachea open.
Bronchi:
The trachea divided into two main bronchi. The bronchi extend into the lungs spreading in a tree-like manner as bronchial tubes. The bronchial tubes subdivide and with each subdivision, their walls get thinner. This dividing of the bronchi into thin-walled tubes results in the formation of bronchioles. The bronchioles terminate in small air chambers, each of which contains cavities known as alveoli. Alveoli have thin walls, which form the respiratory surface. The exchange of gases between the blood and the air takes place through these walls.
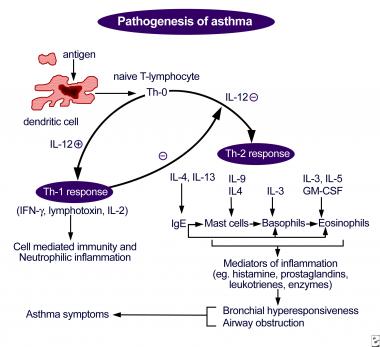
PATHOPHYSIOLOGY
CLINICAL MANIFESTATIONS
| MILD ASTHMA | MODERATE ASTHMA | SEVERE ASTHMA | RESPIRATORY FAILURE |
| Brief wheezing, coughing, dyspnea with activity.
|
Respiratory distress at rest. | Marked respiratory distress | Severe respiratory distress |
| Infrequent nocturnal coughing or wheezing | Hypernea | Marked wheezing or absent breath sounds. | Impaired consciousness |
| Adequate air exchange | Marked coughing and wheezing. | Pulsus paradoxus greater than 10 mm Hg | Severe wheezing or silent chest |
| Intermittent brief(less than 1 hour) wheezing cough, or dyspnea, once or twice a week. | Air exchange normal or below normal. | Chest wall contractions | Use of accessory muscles of respiration |
| Asymptomatic between attacks. | Exacerbations that may last several days. | Continuous symptoms. | Prominent pulsus paradoxus (30-50 mm Hg) |
| Possible sleep interruptions. | Frequent exacerbations. | Cyanosis, tachycardia.
|
NURSING MANAGEMENT
- Assess the severity of the asthma
- Administer the prescribed treatments and assess the patient’s response.
- Place the patient in high fowler’s position. Encourage pursed lip and diaphragmatic breathing. Help him to relax.
- Monitor the patient’s vital signs.
- Administer prescribed humidified oxygen by nasal cannula at 2L/minute to ease breathing. Later, adjust oxygen according to patient’s vital signs and ABG levels. Provide nebulization as prescribed.
- Anticipate intubation and mechanical ventilation if the patient fails to maintain adequate oxygenation.
- Observe the patient for signs of ophylline toxicity (vomiting, diarrhea, and headache.) as well as signs for subtherapeutic dosage (respiratory distress and increased wheezing.)
- Observe the patients frequency and severity of the patients cough, and note whether it’s productive. Then auscultate his lungs, noting adventitious or absent sounds. Teach him effective coughing techniques. Suction an intubated patient as needed.
- Treat dehydration with IV fluids until the patient can tolerate oral fluids, which will help loosen secretions.
During long term-care:
- Monitor the patient’s respiratory status to detect baseline changes, to assess response to treatment, and to prevent or detect complications.
- Auscultate the lungs frequently, noting the degree of wheezing and quality of air movement.
- Review ABG levels, pulmonary function test results, and SaO₂ readings.
- If the patient is taking systematic corticosteroids, observe for complications such as elevated blood glucose levels, and friable skin and bruising.
- Observe the patients anxiety level.
- Keep the room temperature comfortable and use an air conditioner or a fan in hot, humid weather.
For all patients:
- Teach the patient and his family avoid known allergens and irritants.
- Describe prescribe drugs including their names, dosages, actions, adverse effect and special instructions.
- Teach the patient how to use a metered-dose inhaler. If he has difficulty using an inhaler, he may need an extender device to optimize drug delivery and lower the risk of candidal infection with orally inhaled corticosteroids.
- If the patient has moderate to severe asthma, explain how to use a peak flow meter to measure the degree of airway obstruction. Tell him how to keep record of peak flow readings and to bring it to medical appointments. Explain the importance of calling the doctor at once if the peak flow drops suddenly. (a drop can signal severe respiratory problems.)
- Tell the patient to notify the doctor if he develops a fever higher than 100°F (37.8°C), chest pain, shortness of breath, without coughing or exercising, or uncontrollable coughing. An uncontrollable asthma attack requires immediate attention.
- Teach the patient diaphragmatic and pursed-lip breathing as well as effective techniques.
- Urge the patient to drink at least 3L of fluids daily to help loosen secretions and maintain hydration.
MEDICAL MANAGEMENT
- Medications are used in a stepwise fashion, with additional therapies added as needed.
- Inhaled beta-agonist bronchodilators—first-line therapy; used for maintenance and increased with acute attacks.
- Inhaled corticosteroids- added for exacerbations and may be needed for maintenance therapy in moderate asthma.
- Oral corticosteroids and oral-beta agonist or methylxanthine bronchodilators are added as secondary line therapy for moderate to severe asthma.
- Inhaled cholinergics may be tried if condition is unresponsive to beta-agonists.
- Immunotherapy – desensitization of immune system to a known allergen (s) that causes type I (immediate) hypersensitivity.
For STATUS ASTHMATICUS
- Treatment consists of aggressive drug therapy: a beta-adrenergic agonist by nebulizer every 30 to 60 minutes possibly supplemented with S.C. epinephrine, IV corticosteroids, IV aminophylline, oxygen administration, IV fluid therapy, and intubation and mechanical ventilation for hypercapnic respiratory failure (PaCo2 of 40 mmHg or more).