Corynebacteria are Gram-positive, aerobic, nonmotile, rod-shaped bacteria related to the Actinomycetes. They do not form spores or branch as do the actinomycetes, but they have the characteristic of forming irregular shaped, club-shaped or V-shaped arrangements in normal growth. They undergo snapping movements just after cell division which brings them into characteristic arrangements resembling Chinese letters. The genus Corynebacterium consists of a diverse group of bacteria including animal and plant pathogens, as well as saprophytes. Some corynebacteria are part of the normal flora of humans, finding a suitable niche in virtually every anatomic site. The best known and most widely studied species is Corynebacterium diphtheriae, the causal agent of the disease diphtheria.
History and Background
No bacterial disease of humans has been as successfully studied as diphtheria. The etiology, mode of transmission, pathogenic mechanism and 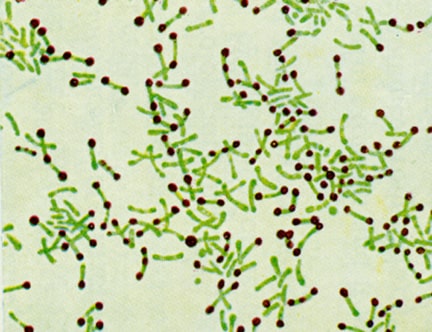 molecular basis of exotoxin structure, function, and action have been clearly established. Consequently, highly effective methods of treatment and prevention of diphtheria have been developed. The study of Corynebacterium diphtheriae traces closely the development of medical microbiology, immunology and molecular biology. Many contributions to these fields, as well as to our understanding of host-bacterial interactions, have been made studying diphtheria and the diphtheria toxin. Hippocrates provided the first clinical description of diphtheria in the 4th century B.C. There are also references to the disease in ancient Syria and Egypt. In the 17th century, murderous epidemics of diphtheria swept Europe; in Spain “El garatillo” (the strangler”), in Italy and Sicily, “the gullet disease”. In the 18th century, the disease reached the American colonies and reached epidemic proportions in 1735. Often, whole families died of the disease in a few weeks. The bacterium that caused diphtheria was first described by Klebs in 1883, and was cultivated by Loeffler in 1884, who applied Koch’s postulates and properly identified Corynebacterium diphtheriae as the agent of the disease. In 1884, Loeffler concluded that C. diphtheriae produced a soluble toxin, and thereby provided the first description of a bacterial exotoxin. In 1888, Roux and Yersin demonstrated the presence of the toxin in the cell-free culture fluid of C. diphtheriae which, when injected into suitable lab animals, caused the systemic manifestation of diphtheria. Two years later, von Behring and Kitasato succeeded in immunizing guinea pigs with a heat-attenuated form of the toxin and demonstrated that the sera of immunized animals contained an antitoxin capable of protecting other susceptible animals against the disease. This modified toxin was suitable for immunizing animals to obtain antitoxin but was found to cause severe local reactions in humans and could not be used as a vaccine. In 1909, Theobald Smith, in the U.S., demonstrated that diphtheria toxin neutralized by antitoxin (forming a Toxin-Anti-Toxin complex, TAT) remained immunogenic and eliminated local reactions seen in the modified toxin. For some years, beginning about 1910, TAT was used for active immunization against diphtheria. TAT had two undesirable characteristics as a vaccine. First, the toxin used was highly toxic, and the quantity injected could result in a fatal toxemia unless the toxin was fully neutralized by antitoxin. Second, the antitoxin mixture was horse serum, the components of which tended to be allergenic and to sensitize individuals to the serum. In 1913, Schick designed a skin test as a means of determining susceptibility or immunity to diphtheria in humans. Diphtheria toxin will cause an inflammatory reaction when very small amounts are injected intracutaneously. The Schick Test involves injecting a very small dose of the toxin under the skin of the forearm and evaluating the injection site after 48 hours. A positive test (inflammatory reaction) indicates susceptibility (nonimmunity). A negative test (no reaction) indicates immunity (antibody neutralizes toxin). In 1929, Ramon demonstrated the conversion of diphtheria toxin to its nontoxic, but antigenic, equivalent (toxoid) by using formaldehyde. He provided humanity with one of the safest and surest vaccines of all time-the diphtheria toxoid. In 1951, Freeman made the remarkable discovery that pathogenic (toxigenic) strains of C. diphtheriae are lysogenic, (i.e., are infected by a temperate B phage), while non lysogenized strains are avirulent. Subsequently, it was shown that the gene for toxin production is located on the DNA of the B phage. In the early 1960s, Pappenheimer and his group at Harvard conducted experiments on the mechanism of an action of the diphtheria toxin. They studied the effects of the toxin in HeLa cell cultures and in cell-free systems, and concluded that the toxin inhibited protein synthesis by blocking the transfer of amino acids from tRNA to the growing polypeptide chain on the ribosome. They found that this action of the toxin could be neutralized by prior treatment with diphtheria antitoxin. Subsequently, the exact mechanism of action of the toxin was shown, and the toxin has become a classic model of a bacterial exotoxin.
molecular basis of exotoxin structure, function, and action have been clearly established. Consequently, highly effective methods of treatment and prevention of diphtheria have been developed. The study of Corynebacterium diphtheriae traces closely the development of medical microbiology, immunology and molecular biology. Many contributions to these fields, as well as to our understanding of host-bacterial interactions, have been made studying diphtheria and the diphtheria toxin. Hippocrates provided the first clinical description of diphtheria in the 4th century B.C. There are also references to the disease in ancient Syria and Egypt. In the 17th century, murderous epidemics of diphtheria swept Europe; in Spain “El garatillo” (the strangler”), in Italy and Sicily, “the gullet disease”. In the 18th century, the disease reached the American colonies and reached epidemic proportions in 1735. Often, whole families died of the disease in a few weeks. The bacterium that caused diphtheria was first described by Klebs in 1883, and was cultivated by Loeffler in 1884, who applied Koch’s postulates and properly identified Corynebacterium diphtheriae as the agent of the disease. In 1884, Loeffler concluded that C. diphtheriae produced a soluble toxin, and thereby provided the first description of a bacterial exotoxin. In 1888, Roux and Yersin demonstrated the presence of the toxin in the cell-free culture fluid of C. diphtheriae which, when injected into suitable lab animals, caused the systemic manifestation of diphtheria. Two years later, von Behring and Kitasato succeeded in immunizing guinea pigs with a heat-attenuated form of the toxin and demonstrated that the sera of immunized animals contained an antitoxin capable of protecting other susceptible animals against the disease. This modified toxin was suitable for immunizing animals to obtain antitoxin but was found to cause severe local reactions in humans and could not be used as a vaccine. In 1909, Theobald Smith, in the U.S., demonstrated that diphtheria toxin neutralized by antitoxin (forming a Toxin-Anti-Toxin complex, TAT) remained immunogenic and eliminated local reactions seen in the modified toxin. For some years, beginning about 1910, TAT was used for active immunization against diphtheria. TAT had two undesirable characteristics as a vaccine. First, the toxin used was highly toxic, and the quantity injected could result in a fatal toxemia unless the toxin was fully neutralized by antitoxin. Second, the antitoxin mixture was horse serum, the components of which tended to be allergenic and to sensitize individuals to the serum. In 1913, Schick designed a skin test as a means of determining susceptibility or immunity to diphtheria in humans. Diphtheria toxin will cause an inflammatory reaction when very small amounts are injected intracutaneously. The Schick Test involves injecting a very small dose of the toxin under the skin of the forearm and evaluating the injection site after 48 hours. A positive test (inflammatory reaction) indicates susceptibility (nonimmunity). A negative test (no reaction) indicates immunity (antibody neutralizes toxin). In 1929, Ramon demonstrated the conversion of diphtheria toxin to its nontoxic, but antigenic, equivalent (toxoid) by using formaldehyde. He provided humanity with one of the safest and surest vaccines of all time-the diphtheria toxoid. In 1951, Freeman made the remarkable discovery that pathogenic (toxigenic) strains of C. diphtheriae are lysogenic, (i.e., are infected by a temperate B phage), while non lysogenized strains are avirulent. Subsequently, it was shown that the gene for toxin production is located on the DNA of the B phage. In the early 1960s, Pappenheimer and his group at Harvard conducted experiments on the mechanism of an action of the diphtheria toxin. They studied the effects of the toxin in HeLa cell cultures and in cell-free systems, and concluded that the toxin inhibited protein synthesis by blocking the transfer of amino acids from tRNA to the growing polypeptide chain on the ribosome. They found that this action of the toxin could be neutralized by prior treatment with diphtheria antitoxin. Subsequently, the exact mechanism of action of the toxin was shown, and the toxin has become a classic model of a bacterial exotoxin.
Human Disease
Diphtheria is a rapidly developing, acute, febrile infection which involves both local and systemic pathology. A local lesion develops in the  upper respiratory tract and involves necrotic injury to epithelial cells. As a result of this injury, blood plasma leaks into the area and a fibrin network forms which is interlaced with with rapidly- growing C. diphtheriae cells. This membranous network covers over the site of the local lesion and is referred to as the pseudomembrane. The diphtheria bacilli do not tend to invade tissues below or away from the surface epithelial cells at the site of the local lesion. At this site they produce the toxin that is absorbed and disseminated through lymph channels and blood to the susceptible tissues of the body. Degenerative changes in these tissues, which include heart, muscle, peripheral nerves, adrenals, kidneys, liver and spleen, result in the systemic pathology of the disease. In parts of the world where diphtheria still occurs, it is primarily a disease of children, and most individuals who survive infancy and childhood have acquired immunity to diphtheria. In earlier times, when nonimmune populations (i.e., Native Americans) were exposed to the disease, people of all ages were infected and killed.
upper respiratory tract and involves necrotic injury to epithelial cells. As a result of this injury, blood plasma leaks into the area and a fibrin network forms which is interlaced with with rapidly- growing C. diphtheriae cells. This membranous network covers over the site of the local lesion and is referred to as the pseudomembrane. The diphtheria bacilli do not tend to invade tissues below or away from the surface epithelial cells at the site of the local lesion. At this site they produce the toxin that is absorbed and disseminated through lymph channels and blood to the susceptible tissues of the body. Degenerative changes in these tissues, which include heart, muscle, peripheral nerves, adrenals, kidneys, liver and spleen, result in the systemic pathology of the disease. In parts of the world where diphtheria still occurs, it is primarily a disease of children, and most individuals who survive infancy and childhood have acquired immunity to diphtheria. In earlier times, when nonimmune populations (i.e., Native Americans) were exposed to the disease, people of all ages were infected and killed.
Pathogenicity
The pathogenicity of Corynebacterium diphtheriae includes two distinct phenomena: 1.Invasion of the local tissues of the throat, which requires colonization and subsequent bacterial proliferation. Nothing is known about the adherence mechanisms of this pathogen. 2.Toxigenesis: bacterial production of the diphtheria toxin. The virulence of C. diphtheriae cannot be attributed to toxigenicity alone, since a distinct invasive phase apparently precedes toxigenesis. However, it cannot be ruled out that the diphtheria toxin plays a (essential?) role in the colonization process due to its short-range effects at the colonization site. Three strains of Corynebacterium diphtheriae are recognized, gravis, intermedius and mitis. They are listed here by falling order of the severity of the disease that they produce in humans. All strains produce the identical toxin and are capable of colonizing the throat. The differences in virulence between the three strains can be explained by their differing abilities to produce the toxin in rate and quantity, and by their differing growth rates. The gravis strain has a generation time (in vitro) of 60 minutes; the intermedius strain has a generation time of about 100 minutes; and the mitis stain has a generation time of about 180 minutes. The faster growing strains typically produce a larger colony on most growth media. In the throat (in vivo), a faster growth rate may allow the organism to deplete the local iron supply more rapidly in the invaded tissues, thereby allowing earlier or greater production of the diphtheria toxin. Also, if the kinetics of toxin production follow the kinetics of bacterial growth, the faster growing variety would achieve an effective level of toxin before the slow growing varieties.
Toxigenicity
Two factors have great influence on the ability of Corynebacterium diphtheriae to produce the diphtheria toxin: (1) low extracellular concentrations of iron and (2) the presence of a lysogenic prophage in the bacterial chromosome. The gene for toxin production occurs on the chromosome of the prophage, but a bacterial repressor protein controls the expression of this gene. The repressor is activated by iron, and it is in this way that iron influences toxin production. High yields of toxin are synthesized only by lysogenic bacteria under conditions of iron deficiency. The role of iron. In artificial culture the most important factor controlling yield of the toxin is the concentration of inorganic iron (Fe++ or Fe+++) present in the culture medium. Toxin is synthesized in high yield only after the exogenous supply of iron has become exhausted (This has practical importance for the industrial production of toxin to make toxoid. Under the appropriate conditions of iron starvation, C. diphtheriae will synthesize diphtheria toxin as 5% of its total protein!). Presumably, this phenomenon takes place in vivo as well. The bacterium may not produce maximal amounts of toxin until the iron supply in tissues of the upper respiratory tract has become depleted. It is the regulation of toxin production in the bacterium that is partially controlled by iron. The tox gene is regulated by a mechanism of negative control wherein a repressor molecule, product of the DtxR gene, is activated by iron. The active repressor binds to the tox gene operator and prevents transcription. When iron is removed from the repressor (under growth conditions of iron limitation), derepression occurs, the repressor is inactivated and transcription of the tox genes can occur. Iron is referred to as a corepressor since it is required for repression of the toxin gene. The role of B-phage. Only those strains of Corynebacterium diphtheriae that that are lysogenized by a specific Beta-phage produce diphtheria toxin. A phage lytic cycle is not necessary for toxin production or release. The phage contains the structural gene for the toxin molecule, since lysogeny by various mutated Beta phages leads to production of nontoxic but antigenically-related material (called CRM for “cross-reacting material”). CRMs have shorter chain length than the diphtheria toxin molecule but cross react with diphtheria antitoxins due to their antigenic similarities to the toxin. The properties of CRMs established beyond a doubt that the tox genes resided on the phage chromosome rather than the bacterial chromosome. Even though the tox gene is not part of the bacterial chromosome the regulation of toxin production is under bacterial control since the DtxR (regulatory) gene is on bacterial chromosome and toxin production depends upon bacterial iron metabolism. It is of some interest to speculate on the role of the diphtheria toxin in the natural history of the bacterium. Of what value should it be to an organism to synthesize up to 5% of its total protein as a toxin that specifically inhibits protein synthesis in eukaryotes (and archaebacteria)? Possibly the toxin assists colonization of the throat (or skin) by killing epithelial cells or neutrophils. There is no evidence to suggest a key role of the toxin in the life cycle of the organism. Since mass immunization against diphtheria has been practiced, the disease has virtually disappeared, and C. diphtheriae is no longer a component of the normal flora of the human throat and pharynx. It may be that the toxin played a key role in the colonization of the throat in nonimmune individuals and, as a consequence of exhaustive immunization, toxigenic strains have become virtually extinct.
Mode of Action of the Diphtheria Toxin
The diphtheria toxin is a two component bacterial exotoxin synthesized as a single polypeptide chain containing an A (active) domain and a B (binding) domain. Proteolytic nicking of the secreted form of the toxin separates the A chain from the B chain The toxin binds to a specific receptor (now known as the HB-EGF receptor) on susceptible cells and enters by receptor-mediated endocytosis. Acidification of the endosome vesicle results in unfolding of the protein and insertion of a segment into the endosomal membrane. Apparently as a result of activity on the endosome membrane, the A subunit is cleaved and released from the B subunit as it inserts and passes through the membrane. Once in the cytoplasm, the A fragment regains its conformation and its enzymatic activity. Fragment A catalyzes the transfer of ADP-ribose from NAD to the eukaryotic Elongation Factor 2 which inhibits the function of the latter in protein synthesis. Ultimately, inactivation of all of the host cell EF-2 molecules causes death of the cell. Attachment of the ADP ribosyyl group occurs at an unusual derivative of histadine called diphthamide.
Mode of Action of the Diphtheria Toxin
In vitro, the native diphtheria toxin is inactive and can be activated by trypsin in the presence of thiol. The enzymatic activity of fragment A is masked in the intact toxin. Fragment B is required to bind the native toxin to its cognate receptor and to permit the escape of fragment A from the endosome. The C terminal end of Fragment B contains the peptide region that attaches to the HB-EGF receptor on the sensitive cell membrane, and the N-terminal end is a strongly hydrophobic region which will insert into a membrane lipid bilayer. The specific membrane receptor, heparin-binding epidermal growth factor (HB-EGF) precursor is a protein on the surface of many types of cells. The occurrence and distribution of the HB-EGF receptor on cells determines the susceptibility of an animal species, and certain cells of an animal species, to the diphtheria toxin. Normally, the HB- EGF precursor releases a peptide hormone that influences normal cell growth and differentiation. One hypothesis is that the HB-EGF receptor itself is the protease that nicks the A fragment and reduces the disulfide bridge between it and the B fragment when the A fragment makes its way through the endosomal membrane into the cytoplasm.
Immunity to Diphtheria
Acquired immunity to diphtheria is due primarily to toxin-neutralizing antibody (antitoxin). Passive immunity in utero is acquired transplacentally and can last at most 1 or 2 years after birth. In areas where diphtheria is endemic and mass immunization is not practiced, most young children are highly susceptible to infection. Probably active immunity can be produced by a mild or inapparent infection in infants who retain some maternal immunity, and in adults infected with strains of low virulence (inapparent infections). Individuals that have fully recovered from diphtheria may continue to harbor the organisms in the throat or nose for weeks or even months. In the past, it was mainly through such healthy carriers that the disease was spread, and toxigenic bacteria were maintained in the population. Before mass immunization of children, carrier rates of C. diphtheriae of 5% or higher were observed. Because of the high degree of susceptibility of children, artificial immunization at an early age is universally advocated. Toxoid is given in 2 or 3 doses (1 month apart) for primary immunization at an age of 3 – 4 months. A booster injection should be given about a year later, and it is advisable to administer several booster injections during childhood. Usually, infants in the United States are immunized with a trivalent vaccine containing diphtheria toxoid, pertussis vaccine, and tetanus toxoid (DPT or DTP vaccine).
