In the emergency setting, anaphylaxis is a dangerous, life threatening condition that must be treated in an aggressive and timely fashion. Anaphylaxis is a condition related to acute allergic reactions. Following the body’s exposure to the offending allergen, there are common systemic reactions.
The most serious reactions involve the respiratory and cardiovascular systems, but the gastrointestinal, dermatologic, and 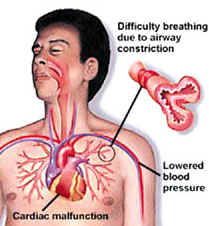 genitourinary systems are often involved causing varied symptoms such as urticaria, flushing, angioedema, bronchospasm, hypotension, cardiac arrythmias, nausea, intestinal cramps, pruritus, and finally uterine cramps. (Physician Assistant, 8/94) The above list is by no means exhaustive, specific symptoms vary from person to person. The same person suffering from several anaphylactic reactions can also present with differing symptoms.
genitourinary systems are often involved causing varied symptoms such as urticaria, flushing, angioedema, bronchospasm, hypotension, cardiac arrythmias, nausea, intestinal cramps, pruritus, and finally uterine cramps. (Physician Assistant, 8/94) The above list is by no means exhaustive, specific symptoms vary from person to person. The same person suffering from several anaphylactic reactions can also present with differing symptoms.
Physiologically speaking, the two main effects of the body’s released mediators (IgE) during an anaphylactic reaction are smooth muscle contraction and vasodilatation, which cause most of the body’s adverse symptoms. (JAMA, 11/26/82) Since the most life threatening reactions usually involve the respiratory and cardiovascular systems, that is where emergency treatment is focused. In the cardiovascular system, a combination of vasodilatation, increased vascular permeability, tachcycardia, and arrhythmias can lead to severe hypotension. In the respiratory system, the swelling of tissues along with bronchospasm and increased mucus production are the main cause of death. So, if untreated, anaphylaxis can be fatal as a result of the body’s going into what is essentially shock, while simultaneously (and more importantly) being deprived of the oxygen needed to sustain life.
As of today there is one universally accepted treatment for acute anaphylaxis. Epinephrine. Epinephrine is both an alpha and a beta agonist. This makes it the drug optimally suited to treat anaphylaxis. “Epinephrine will increase vascular resistance, reduce vascular permeability, produce bronchodilation and increase cardiac output.” (Emergency, 10/93)
Epinephrine will directly counteract the potentially life threatening aspects of anaphylaxis. Epinephrine can , and is, used in the both the pre-hospital environment as well as in definitive care institutions. Epinephrine is widely administered by ALS providers the world over. The drug is so effective that and relatively simple to use that “…subcutaneous administration of epinephrine by EMT-B’s trained in recognition … of anaphylaxis… is safe.” (Annals of Emergency Medicine, 6/95)
Following the administration of epinephrine, antihistamines such as diphenhydramine, hydroxyzine, and promethazine can be administered. These agents block the harmful effects of histamine, a mediator associated with allergic reactions, and while not displacing histamine from receptors, they compete with histamine for receptor cites and therefore block additional histamine from binding. (JEMS, 4/95)
Patients taking beta adrenergic blocking agents will have limited benefits from the administration of epinephrine (it being a beta agent), as well potentially unopposed alpha adrenergic effects that could result in severe hypertension. (Physician Assistant, 8/94) In such cases norepinepherine and dopamine may be necessary to treat systemic anaphylaxis. Glucagon which increases cAMP, is a bronchodilator, and stimulates cardiac output, can be very useful, even in the presence of beta blockers. (Physician Assistant, 8/94)
Inhaled bronchodilators are useful for the treatment of respiratory complications associated with anaphylaxis. There is a wide variety of acceptable agents. Sympathomimetics such as albuterol, and metaproterenol will relax the smooth muscle in the respiratory tract. Anticholinergic agents such as ipratropium bromide can also decrease bronchospasm. Aminophylline, a bronchodilator and diuretic can also increase intracellular cAMP levels, as well as potentiating catecholamines and stimulating their release; these effects make it a useful tool in dealing with persistent bronchospasm. (Physician Assistant, 8/94)
Even though steroids (glucocorticosteroids) have some potentially beneficial effects for the relief of bronchospasm and hypotension, they are not recommended for the treatment of acute anaphylactic symptoms due to the fact that it takes four to six hours for them to be effective. (JAMA, 11/26/82) But, steroids such as methylprednisolone and hydrocortisone, are useful in shortening the duration of, and reducing the severity of prolonged anaphylactic reactions, as well as preventing the recurrence of delayed symptoms. (Physician Assistant, 8/94)
The above agents are all widely used to treat anaphylaxis. But there are studies and experiments underway that are looking at alternative, or additional treatments. Naloxone and thyrotropin-releasing hormone (TRH) are both being looked at in the possible treatment of anaphylaxis as well as traumatic shock. “Naloxone improves cardiovascular function in a variety of animal models of shock caused by…and anaphylaxis. Administration of TRH …also has pressor effects in these shock models.” (Annals of Emergency Medicine, 8/85)
“TRH has been shown to increase mean arterial pressure during anaphylactic shock.” (Annals of Emergency Medicine, 5/89) In animal studies of anaphylaxis the use of TRH, epinephrine, and normal saline were compared. TRH treated rabbits responded slightly better than those treated with epinephrine (the study focused on cardiovascular and respiratory parameters.) (Annals of Emergency Medicine, 5/89)
